Introduction
Patient adherence, often referred to as medication adherence or compliance, is a critical component in the healthcare sector. It encapsulates how patients accurately follow prescribed medical treatments from their healthcare providers. Beyond taking medications correctly, this concept encompasses various facets of a treatment plan, extending beyond dosage and timing.
For instance, it includes adhering to dietary recommendations provided by healthcare professionals. These could range from general advice about maintaining a balanced diet to specific instructions related to the patient’s condition. Such as limiting sodium intake for patients with hypertension or avoiding certain foods for those with allergies.
Exercise regimens are another crucial part of patient adherence. Regular physical activity can help manage many health conditions and prevent health issues such as heart disease and diabetes. Therefore, following prescribed exercise routines forms an integral part of treatment plans for many patients.
Lifestyle changes also fall under the umbrella of patient adherence. These can encompass a wide variety of modifications in a person’s daily routine. Such as quitting smoking, reducing alcohol consumption, or getting adequate sleep. These changes can significantly impact a patient’s health outcomes and are therefore an essential part of their treatment plan.
In essence, patient adherence is a multifaceted concept that goes beyond just taking medications correctly. It involves a holistic approach to healthcare, incorporating medication use, diet, exercise, and lifestyle changes. As such, it plays a role in determining the effectiveness of treatment plans and contributes to improved patient health outcomes.
Importance of Patient Adherence

The importance of patient adherence cannot be overstated. When patients adhere to their treatment plans, they increase their chances of achieving optimal health outcomes. This is true for chronic conditions such as diabetes, hypertension, and heart disease. Where long-term medication use and lifestyle changes can significantly improve health outcomes and quality of life.
Moreover, patient adherence can lead to a reduction in healthcare costs. Non-adherence often results in worsening health conditions that require more intensive and costly treatments. For example, a patient with hypertension who does not take medication regularly may end up needing hospitalization for a stroke or heart attack. Thus, improving patient adherence can save healthcare systems millions of dollars each year.
Despite its importance, patient adherence is a significant challenge in healthcare. Studies have shown that up to 50% of patients do not take their medications as prescribed. This non-adherence can be intentional, where patients consciously decide not to follow their treatment plan, or unintentional, where patients forget or are unable to follow their treatment plan due to factors such as complex medication regimens or lack of understanding about their condition and treatment.
Several factors contribute to non-adherence. These include patient-related factors (e.g., forgetfulness, lack of motivation), healthcare provider-related factors (e.g., poor communication, lack of patient involvement in treatment decisions), and system-related factors (e.g., high medication costs, lack of access to care).
Addressing non-adherence requires a multifaceted approach. Interventions can range from patient education and counseling to improve understanding and motivation, to the use of technology such as medication reminders and telehealth services to support adherence. Healthcare providers also play a critical role in promoting adherence by building trusting relationships with patients, involving them in treatment decisions, and providing clear instructions about medication use.
Patient adherence is a complex but vital aspect of healthcare that has significant implications for patient health outcomes and healthcare costs. While non-adherence is a common problem, it can be addressed through various strategies that involve patients, healthcare providers, and the healthcare system as a whole.
Benefits of Personalized Rx Programs
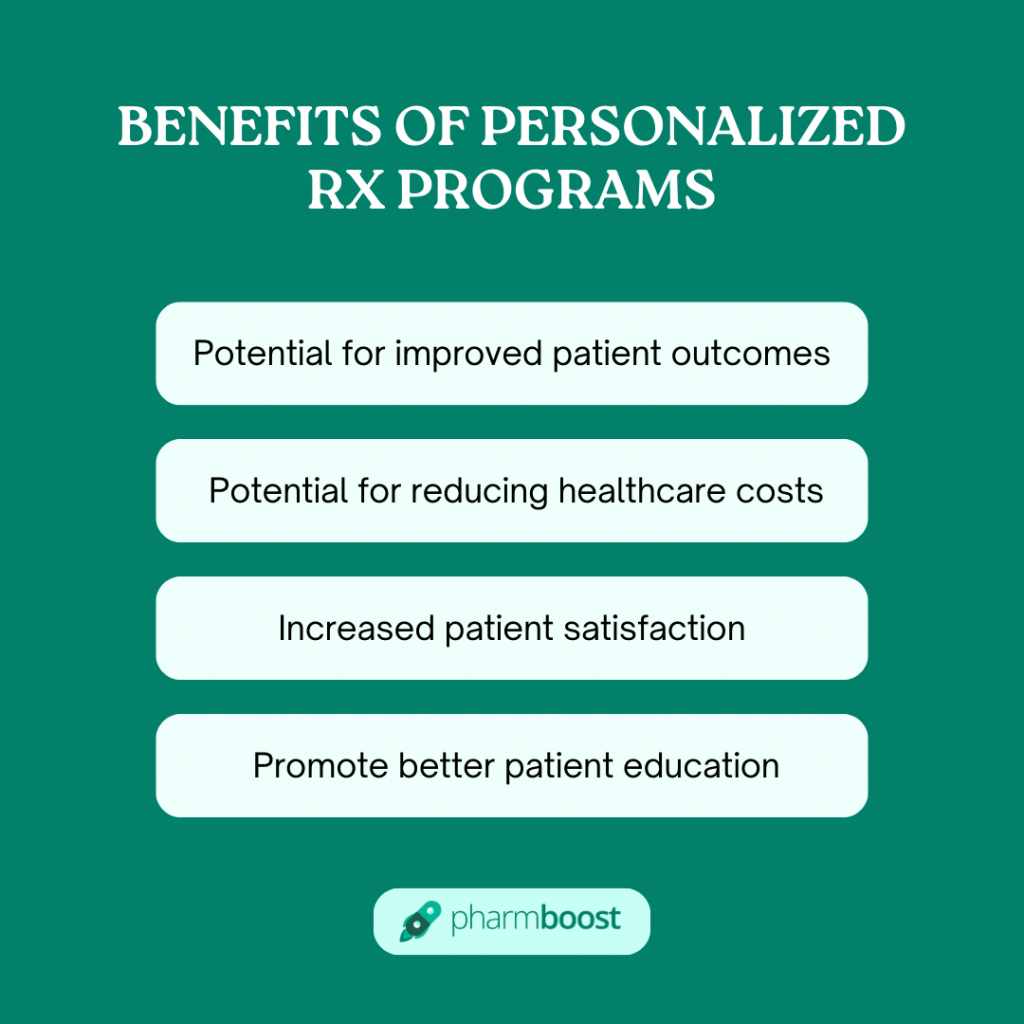
Personalized Rx programs, also known as personalized prescription programs, are a revolutionary approach in the healthcare sector designed to enhance patient adherence to medication regimens. These programs are tailored to meet the unique needs of each patient, taking into account their specific health conditions, lifestyle, and personal preferences. The benefits of these programs are manifold, ranging from improved patient outcomes to reduced healthcare costs and increased patient satisfaction.
One of the primary benefits of Personalized Rx programs is the potential for improved patient outcomes. By customizing treatment plans to suit individual patient needs, these programs can increase the effectiveness of medications and reduce the risk of adverse drug reactions. This personalized approach ensures that patients receive the right medication at the right dose and at the right time, thereby maximizing therapeutic benefits and minimizing potential harm.
Another significant advantage of Personalized Rx programs is the potential for reducing healthcare costs. Non-adherence to medication regimens is a prevalent issue that leads to increased hospitalizations and healthcare expenditures. By improving medication adherence, Personalized Rx programs can help prevent unnecessary hospital admissions and reduce the burden on healthcare systems. Moreover, by optimizing medication use, these programs can also decrease wastage and lower prescription drug costs.
Increased patient satisfaction is another key benefit of Personalized Rx programs. Patients are more likely to adhere to their medication regimens when they feel understood and involved in their treatment decisions. Personalized Rx programs foster this sense of involvement by taking into account patient preferences and lifestyle factors when designing treatment plans. This patient-centric approach can enhance patient satisfaction and improve overall quality of life.
Furthermore, Personalized Rx programs can also promote better patient education and empowerment. These programs often involve regular interactions between patients and healthcare providers, providing opportunities for patients to learn more about their health conditions and treatment options. This increased knowledge can empower patients to take an active role in managing their health and make informed decisions about their care.
Personalized Rx programs offer numerous benefits that can transform healthcare delivery. By promoting medication adherence, improving patient outcomes, reducing healthcare costs, increasing patient satisfaction, and empowering patients, these programs hold great promise for enhancing the quality and efficiency of healthcare.
How to Create Personalized Rx Programs
Creating personalized Rx programs is a complex process that requires a multidisciplinary approach involving healthcare providers, pharmacists, and patients. The goal is to ensure that patients receive the most effective treatment for their specific needs, while also promoting medication adherence. Here are some steps to create effective personalized Rx programs:
- Identifying At-Risk Patients
The first step in creating a personalized Rx program is identifying patients who are at risk for non-adherence. Factors such as age, comorbidities, and medication complexity can all contribute to a patient’s likelihood of not adhering to their medication regimen. By identifying these patients early, healthcare providers can intervene and provide additional support to promote adherence. - Developing Personalized Treatment Plans
Once at-risk patients have been identified, healthcare providers should work with them to develop personalized treatment plans. These plans should take into account the patient’s individual needs and preferences, as well as any potential barriers to adherence. This might involve choosing medications with fewer side effects, simplifying the dosing schedule, or even changing the medication entirely if it’s not working for the patient. - Providing Education and Support
Education and support are crucial components of any personalized Rx program. Patients need to understand the importance of adherence and how to manage their medications effectively. This can be achieved through regular consultations with healthcare providers and pharmacists, who can provide advice on how to take medications correctly, manage side effects, and address any concerns or questions the patient might have. - Leveraging Technology
Technology can also play a key role in promoting medication adherence. Mobile apps and text messaging services can provide reminders for patients to take their medications, while also offering educational resources to help them better understand their condition and treatment. These tools can be particularly useful for patients with complex medication regimens or those who struggle with forgetfulness.
Creating personalized Rx programs is a collaborative effort that requires input from various healthcare professionals and the patient themselves. By identifying at-risk patients, developing personalized treatment plans, providing education and support, and leveraging technology, healthcare providers can help ensure that patients receive the most effective treatment while also promoting medication adherence.
Strategies for Improving Patient Adherence
Improving patient adherence is a complex task that requires the concerted efforts of healthcare providers, pharmacists, and patients. It is a multifaceted approach that involves several strategies aimed at enhancing the effectiveness of treatment plans and improving patient outcomes.
One of the key strategies is to simplify medication regimens. Healthcare providers should strive to make medication regimens as simple as possible to reduce the burden on patients. This could involve reducing the number of medications a patient needs to take, adjusting the timing of doses to fit with a patient’s daily routine, or using combination medications.
Another strategy is to provide reminders. Reminders can be given by healthcare providers during consultations or through technology such as mobile apps or text messaging. These reminders can help patients remember when to take their medication and can also provide information about the importance of adherence.
Addressing side effects is another crucial strategy. Side effects can be a significant barrier to adherence, so healthcare providers should proactively address any side effects that may be contributing to non-adherence. This could involve adjusting medication doses, switching to a different medication, or providing advice on how to manage side effects.
Finally, healthcare providers should monitor adherence through regular follow-up visits and medication reviews. Regular monitoring can help identify any issues with adherence early on and allows healthcare providers to provide support and interventions as needed.
In conclusion, improving patient adherence requires a comprehensive approach that involves simplifying medication regimens, providing reminders, addressing side effects, and monitoring adherence. By implementing these strategies, healthcare providers can help improve patient outcomes and ensure that patients are receiving the most benefit from their treatment plans.
Conclusion
Patient adherence is indeed a pivotal element in achieving optimal health outcomes and curtailing healthcare costs. Personalized Rx programs, by tailoring treatment plans to individual patient needs, can significantly enhance patient adherence. The creation of effective personalized Rx programs necessitates a multidisciplinary approach that encompasses healthcare providers, pharmacists, and patients. Strategies to bolster patient adherence range from simplifying medication regimens to providing reminders, addressing side effects, and monitoring adherence.
However, the journey to improved patient adherence doesn’t have to be arduous. This is where “Pharmboost” comes into play. “Pharmboost” is a cutting-edge patient engagement solution designed to streamline the process of improving patient adherence. It leverages advanced technology to provide personalized reminders, monitor medication usage, and address potential side effects in real-time.
We invite you to experience the transformative power of “Pharmboost”. Request a demo today and witness firsthand how “Pharmboost” can revolutionize your approach to patient adherence and engagement. Let’s work together to create healthier communities, one patient at a time.
Recent Post
- 5 Actionable Tips to Improve Patient Engagement within 1 Month
- Social Media Check List for Pharmacy Social Media Marketing
- Pharmacy Social Media Marketing 13 dos and don’ts to know
- Patient Engagement Barriers in Your Pharmacy & How Software Can Help You Overcome Them
- How to Attract New Patients and Boost Sales with Local Pharmacy Marketing







